5 Most Common Reasons for Low White Blood Cell Count (Leukopenia)
If you’ve been told you have a low white blood cell count, you’re probably asking: What does that mean for my health? Is it serious? What causes it?
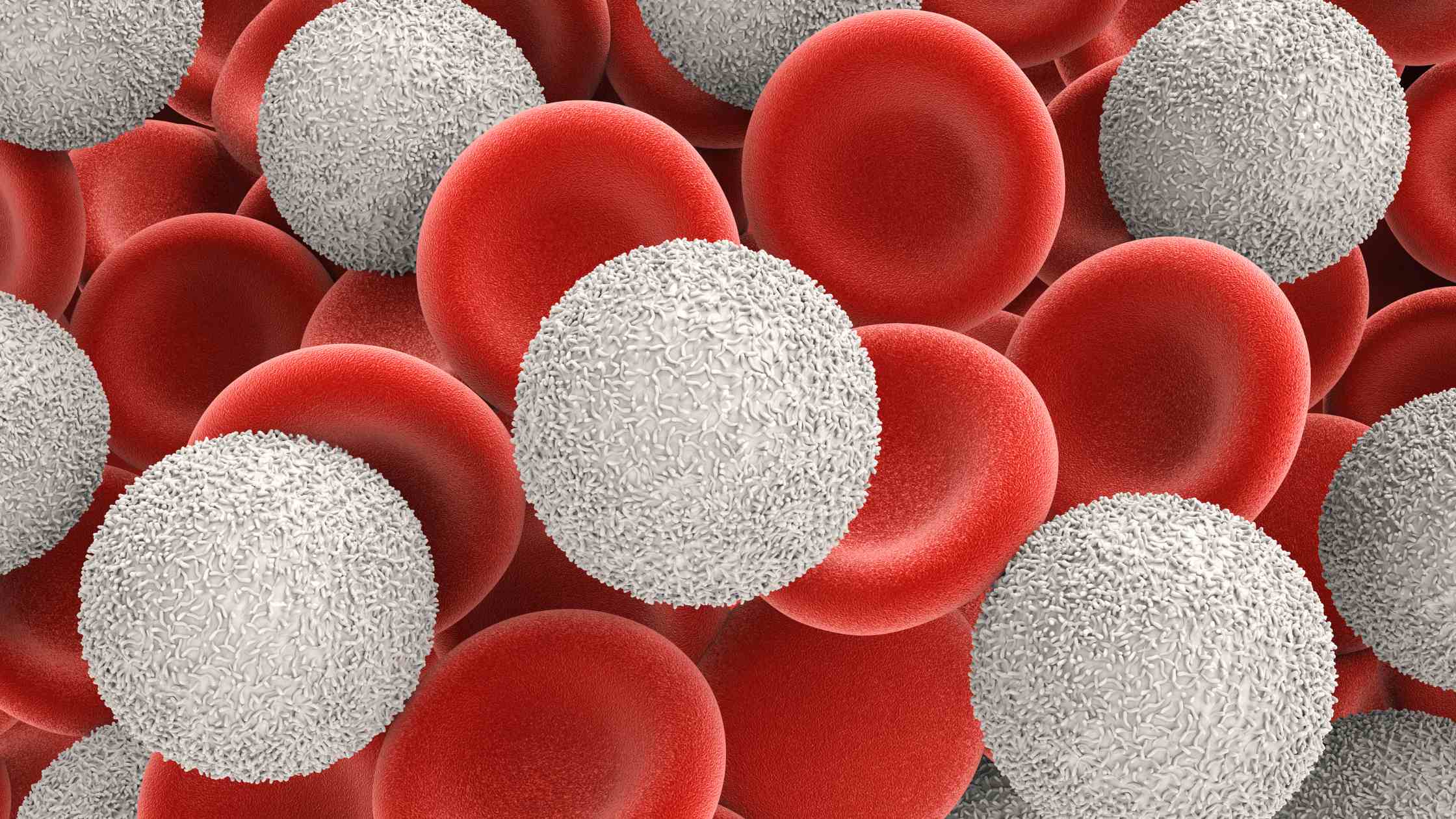
First, let’s clarify—white blood cells (WBCs) are your immune system’s frontline defenders. They fight off infections, respond to inflammation, and protect your body from foreign invaders. So when your white blood cell count drops below normal (a condition called leukopenia), your body becomes more vulnerable to infections and may struggle to heal properly.
A healthy adult typically has a WBC count between 4,500 and 11,000 cells per microliter of blood (according to the Mayo Clinic). When your count falls below that, especially below 4,000, doctors start paying attention. But what’s causing it?
Here are the 5 most common reasons for a low white blood cell count, backed by medical sources and explained in simple terms.
1. Infections (Especially Viral Infections)
Yes, ironically, infections—the very thing your WBCs are supposed to fight—can cause their numbers to drop.
Certain viral infections, like:
- Influenza (flu)
- HIV
- Hepatitis
- COVID-19
…can lead to a temporary suppression of bone marrow, which is where your body produces white blood cells. These viruses either directly damage the bone marrow or redirect your immune response, causing WBC production to drop.
🧠 Fact Check:
According to the Cleveland Clinic, some viruses “slow down bone marrow function or destroy WBCs faster than they can be replaced.”
2. Autoimmune Disorders
Autoimmune diseases like:
- Lupus (SLE)
- Rheumatoid Arthritis
- Sjogren’s Syndrome
…cause your body to mistakenly attack its own white blood cells or bone marrow cells. This misfire leads to fewer white blood cells in circulation.
In my experience as a nurse, I’ve seen patients with lupus have fluctuating WBC levels, especially during flare-ups.
🧠 Medical Note:
The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) confirms that autoimmune diseases can “affect blood cell production and survival.”
3. Cancer and Cancer Treatments (Especially Chemotherapy)
This is a major reason for leukopenia in clinical settings.
Cancers such as:
- Leukemia
- Lymphoma
- Bone marrow cancers
…directly affect the bone marrow’s ability to produce white blood cells.
But even if the cancer isn’t in the blood, chemotherapy and radiation therapy can destroy rapidly dividing cells, including those in the bone marrow.
🧠 Source Insight:
According to Cancer Research UK, “chemotherapy can lower the number of white blood cells in your blood, especially neutrophils, leaving you vulnerable to infections.”
4. Nutritional Deficiencies
Sometimes the cause is as basic as not getting enough of the right nutrients.
Deficiencies in:
- Vitamin B12
- Folate
- Copper
- Zinc
…can lead to poor bone marrow function and lower WBC production. These nutrients are essential for DNA synthesis and cell growth, including white blood cells.
A patient of mine who had chronic gastritis (which affected their B12 absorption) showed improved WBC levels after we corrected their deficiency.
🧠 Reference:
The National Institutes of Health (NIH) notes that both vitamin B12 and folate are vital for healthy blood cell production.
5. Bone Marrow Disorders or Damage
The bone marrow is your WBC factory. When it’s damaged, production of white cells drops drastically.
This can happen because of:
- Aplastic anemia
- Myelodysplastic syndromes
- Radiation exposure
- Toxins (like benzene)
Even chronic conditions like kidney failure can interfere with bone marrow function indirectly.
🧠 Expert Resource:
The American Society of Hematology (ASH) explains that bone marrow disorders are a “primary cause of leukopenia and require thorough evaluation and monitoring.”
Why This Matters
A low white blood cell count shouldn’t be ignored. It doesn’t always mean cancer or a serious autoimmune disorder, but it does signal that something important is happening in your body.
If your count is consistently low, here’s what you should do:
- Talk to your doctor about additional blood tests (CBC with differential, B12 levels, etc.)
- Ask about recent infections, medications, or nutritional habits
- Don’t panic—but don’t ignore it, either
The body’s warning signs aren’t always loud. Sometimes, they show up quietly in lab results. And often, catching the problem early can lead to better outcomes.
Cite this article
You can copy and paste your preferred citation format below.
Martin, L. & Arquette, E.. (2025, May 5). 5 Most Common Reasons for Low White Blood Cell Count (Leukopenia). Coursepivot.com. https://coursepivot.com/blog/5-most-common-reasons-for-low-white-blood-cell-count-leukopenia/



